Healthcare education programs face a shared challenge: building clinical reasoning amid uneven exposure, variable sites, and limited time, where repetition is essential but opportunities and visibility are inconsistent.
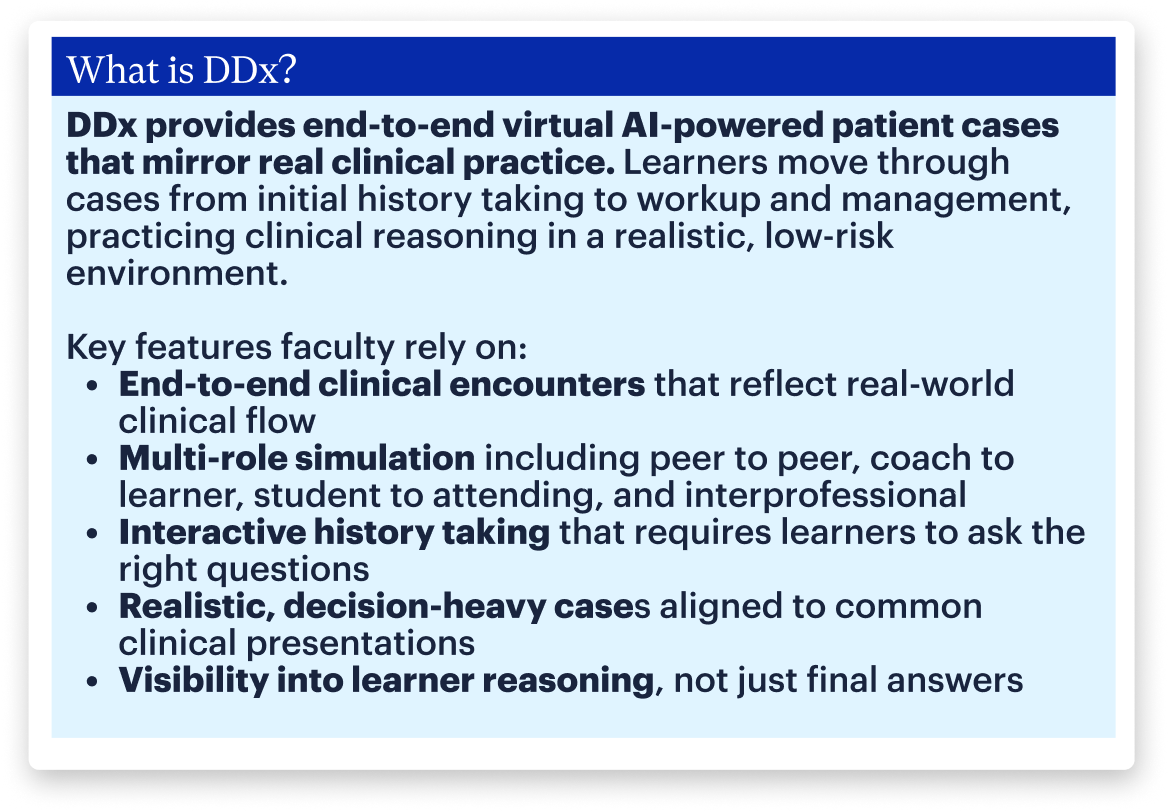
Faculty usage of DDx, an AI-powered virtual case platform, sheds light on the ways programs scale clinical reasoning education. DDx usage data from 2025 reveal these trends in learner behavior and program design.
- Programs take an intentional approach to clinical exposure.
- Learners gravitate toward foundational, high-impact cases to build greater confidence.
- Assigned practice deepens and clarifies student reasoning for faculty.
The insights that follow show how clinical reasoning is being strengthened in practice.
Faculty goals and program design
While program structures vary, faculty across health professions’ education share common goals, balancing limited time, uneven clinical exposure, and the need for consistent clinical reasoning standards.
Engagement data show programs tailor case assignment, timing, and expectations to learner stage and institutional constraints.
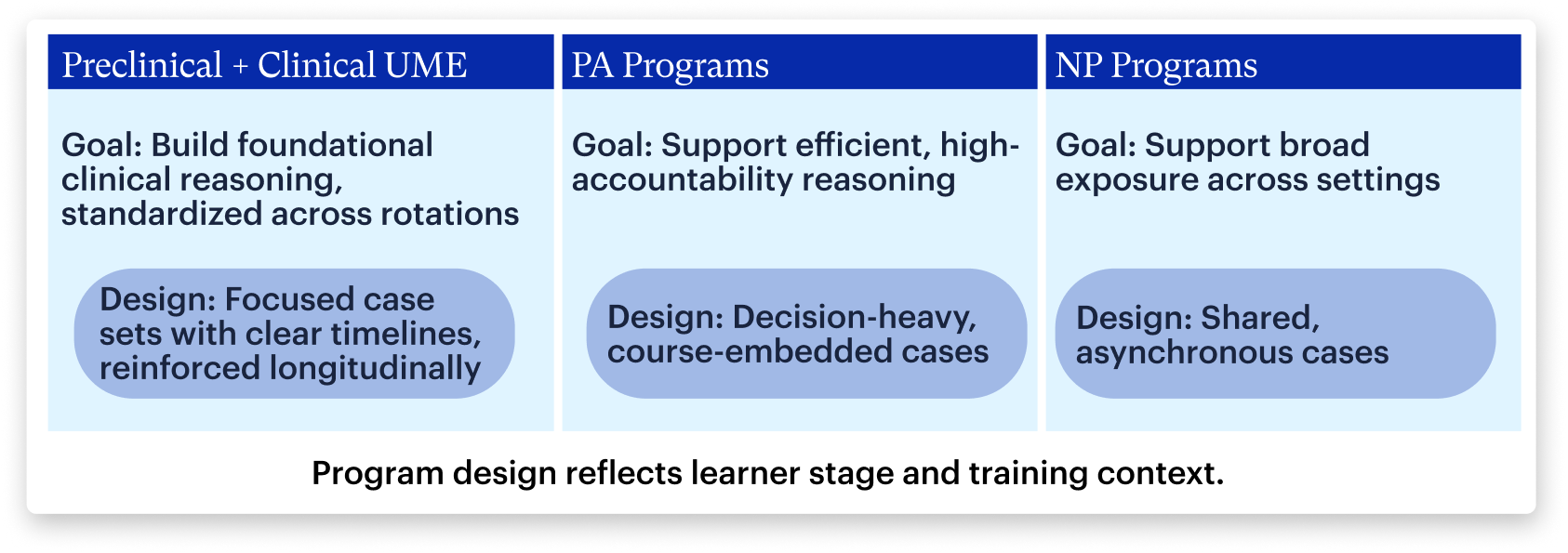
Preclinical UME programs
Goal: Build foundational clinical reasoning habits early without overwhelming learners or disrupting block-based curricula.
Integration:
- Highly curated case assignment: Faculty intentionally assign a focused subset of cases per block, reinforcing that depth and alignment matter more than quantity.
- Case selection: Assigned cases prioritize foundational skills, with 2 of the top 3 featuring interactive physical exams (PE).
- Short completion windows: Time-bound assignments emphasize consistent reasoning, typically within a ~4-week window aligned to block schedules.
Clinical UME programs
Goal: Ensure consistent clinical reasoning across variable rotation sites through shared case-based experiences.
Integration:
- Flexible case engagement: Learners have access to cases tied to curricular milestones, with some programs creating 10+ courses and offering extended access windows.
- Broad library: Learners often engage with 50–75% of the case library, particularly during high-variability rotations.
Targeted assignments for readiness: Faculty assign top cases for OSCE prep and clinical readiness, including cases on chest pain, abdominal pain, accidental ingestion, and fatigue, emphasizing common, high-acuity Emergency and Internal Medicine presentations.
PA programs
Goal: Prepare students to reason efficiently and confidently in a fast-paced, high-accountability clinical training model.
Integration:
- Curated but substantial assignment: Programs assign a meaningful portion of the library, typically 35–40%, balancing structure with efficiency.
- Decision-heavy, longitudinal case focus: Case selection emphasizes common chief complaints, organized across ~10 courses to support repeated, on-demand reasoning practice.
- Integrated, extended access coursework: Assignments are embedded in coursework with extended access windows, reinforcing accountability and longitudinal engagement.
NP programs
Goal: Support broad clinical exposure and consistent clinical reasoning development in asynchronous environments.
Integration:
- Broad case assignment: Commonly assign ~30% of the library, particularly in FNP pathways where exposure breadth is critical.
- Emphasis on primary care presentations: Case selection reflects broad clinical exposure, with 3 of the top 5 assigned cases tied to family or ambulatory rotations. (lower back pain, weight loss, knee pain)
- Shared, asynchronous case integration: Programs assign common cases across sites and schedules to standardize clinical reasoning expectations.
Faculty are making deliberate choices to reflect the realities of modern clinical training, structuring reasoning practice to build habits early, reduce site variability, and maintain consistent expectations. Differences in case selection, timing, and structure reflect learner stage and institutional constraints, not one-size-fits-all adoption.
Where do students need to build more confidence?
Faculty often sense where students struggle, but validating this at scale is difficult due to uneven exposure, leaving confidence gaps hidden until high-stakes settings.
Across all learners, 30% of DDx attempts concentrate around 10 foundational cases out of a 200+ case library. These represent the most in-demand cases, pointing to where students feel the strongest need for repetition.
The most frequently practiced cases center on core chief complaints:
- Fever
- Chest pain
- Abdominal pain
- Shortness of breath
- Hematuria
- Weight loss
- Sore throat
This concentration doesn’t reflect narrow engagement: while 30% of attempts cluster around these cases, the remaining 70% span the broader library, reflecting cross-rotation, high-risk and common presentations.
87% of learners report feeling more confident after completing DDx cases
Together these indicate that repeated, structured practice strengthens both confidence and competence, particularly for high-impact presentations students may not encounter often enough.
Student Voices:
How do student behavior change when cases are assigned?
A core faculty challenge is ensuring students consistently practice safe, complete clinical reasoning, with clear behavioral differences between self-directed and assigned cases.
Across cases, there’s a consistent contrast in student behavior:
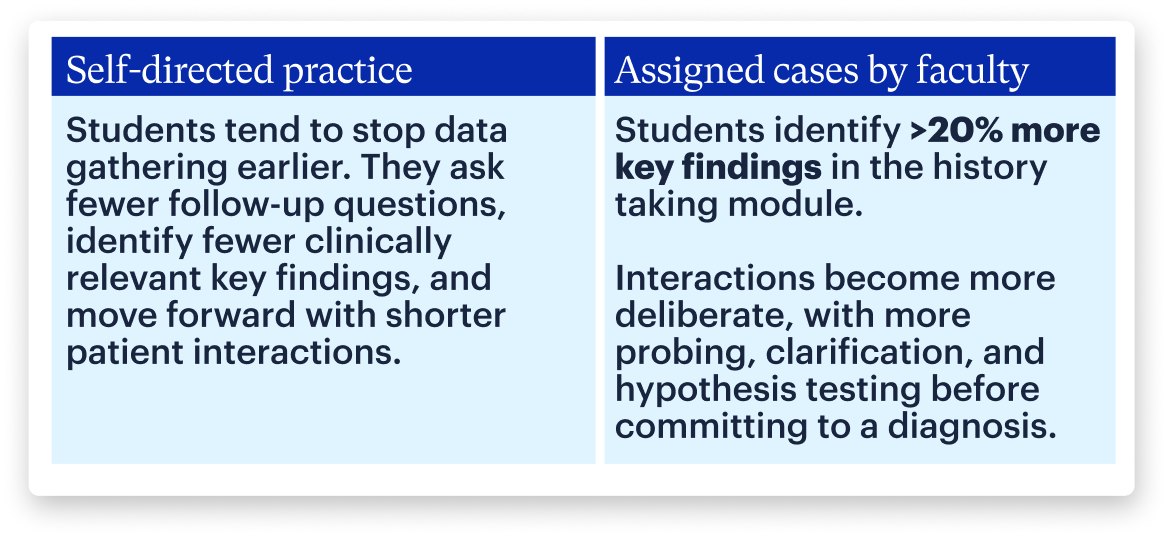
Why this shift matters for faculty
This shift makes clinical reasoning both visible and accountable. Because DDx captures each step of the interaction, faculty can see not just the final answer, but how learners arrive there and whether they apply the expected reasoning process in practice.
This allows faculty to:
- Generate milestone-aligned evidence for coaching and assessment
- Deliver more targeted remediation grounded in observable behavior
- Refine curriculum based on how learners actually reason
Assigned cases reinforce accountability by shifting focus from correctness to reasoning process. When steps are required and visible, students ask better questions, gather fuller data, and build more defensible differentials across clinical settings.
What this means for your program
The data show a clear shift in how clinical reasoning is taught. Faculty are designing experiences that make reasoning visible, comparable, and repeatable across training environments, strengthening confidence and competence without relying on chance exposure.
For programs aiming to strengthen reasoning earlier, reduce variability, or better understand how learners think, these patterns offer a starting point. DDx is one way institutions apply these principles through virtual patient encounters that make reasoning visible and repeatable in practice.
Interested in how this could fit your curriculum? Explore DDx and try a virtual patient case.
